The DC Department of Health (DC Health) strongly recommends the Measles, Mumps, and Rubella (MMR) vaccine, a safe and effective way to prevent measles, a highly contagious disease. Learn more.
To obtain the medical necessity criteria used for a specific service, you may contact Utilization Management.
Fax: (202) 721-7190
Email: UM@hschealth.org
View Prior Authorization Requirements [XLS - 31 KB]
a) Definition of a Medically Necessary Service: A service is Medically Necessary if a physician or other treating health Provider, exercising prudent clinical judgment, would provide or order the service for an Enrollee for the purpose of evaluating, diagnosing or treating illness, injury, disease, physical or mental health conditions, or their symptoms, and the provision of the service is in compliance with 1905(a) of the Act, 42 U.S.C. § 1396d(a), to correct or ameliorate defects and physical and mental illnesses and conditions discovered by the screening services, whether or not such services are covered under the State Plan. Medically Necessary services shall be:
i) No more restrictive than those used in the Medicaid program, including quantitative and non-quantitative treatment limits, as indicated in District statutes and regulations, the State Plan, and other District policy and procedures;
ii) Services and benefits that promote normal growth and development and prevent, diagnose, detect, treat, ameliorate the effects or a physical, mental, behavioral, genetic, or congenital condition, injury, or disability for CASSIP Enrollees;
iii) Provided in accordance with generally accepted standards of medical practice;
iv) Clinically appropriate, in terms of type, frequency, extent, site and duration, and considered effective for the Enrollee’s illness, injury, disease, or physical or behavioral health condition;
v) Not primarily for the convenience of the Enrollee or treating physician, or other treating healthcare Providers, and more cost effective than an alternative service or sequence of services, and at least as likely to produce equivalent therapeutic or diagnostic results with respect to the diagnosis or treatment of that Enrollee’s illness, injury, disease or physical or mental health condition; and Specific to the Enrollee and shall take into account available clinical evidence, as well as recommendations of the treating clinician and other clinical, educational, and social services professionals who treat or interact with the Enrollee.
For services requiring prior authorization, providers must submit requests to the Utilization Management (UM) Department via the following methods:
Non-urgent requests will be addressed within 5 business days.
For Urgent requests requiring immediate attention, please submit your request via:
Urgent requests will be responded to within 24 hours.
Note: Emergency and Stabilization Services (ER Services) never require a prior authorization request regardless of the network status of practitioner, providers or facility providing ER Services.
Out of Network services always require prior authorization. If a provider elects to refer an HSCSN enrollee to a non-participating (out-of-network) provider/specialist for any reason, prior authorization must be obtained from HSCSN before the HSCSN enrollee receives the services.
The following services require notification to the HSCSN Utilization Management Department:
For inpatient admission to a hospital, notification is required within 24 hours of admission. Clinical documents must be submitted by the next business day.
Clinical documents must be submitted by the next business day.
Newborn Deliveries within 24 hours of delivery or the next business day.
Durable Medical Equipment (DME) Delivery Notification
Delivery of Durable Medical Equipment (DME) requires notification to be provided within 24 hours of delivery, or by the next business day.
The following services DO NOT REQUIRE prior authorization when performed by an in-network provider:
The following services DO REQUIRE prior authorization when performed by an in-network provider:
Admission to hospitals for acute care requires concurrent review. The hospital needs to notify HSCSN within 24 hours of admission and subsequent clinicals by the next business day.
HSCSN contracts with CVS/Caremark as our Pharmacy Benefit Manager (PBM). HSCSN delegates utilization management for pharmacy services to the CVS/Caremark Utilization Management Department. CVS/Caremark is responsible for reviewing prior authorization and formulary exception requests for medications dispensed from an outpatient pharmacy and making determinations of medical necessity. HSCSN’s Office of Appeals and Grievances handles all enrollees, and provider appeals and grievances regarding pharmacy services.
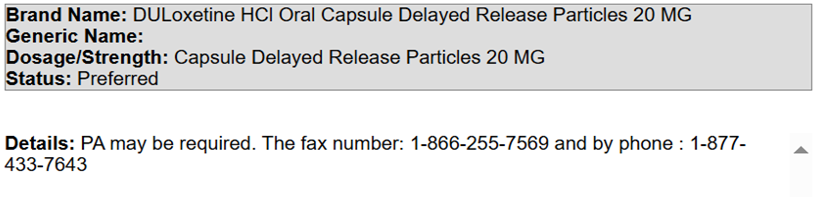
Formulary medications that require prior authorization are indicated in the HSCSN Drug Formulary (see below). Medications that are not on the formulary can be requested as a Formulary Exception through the prior authorization process. Use of a non-formulary medication usually requires that there is no formulary alternative.
A prior authorization request should include the following clinical details for a complete review and decision:
Download the Prior Authorization Request Form
To obtain the medical necessity criteria used for a specific medication, providers may contact Utilization Management at CVS/Caremark.
Requests for prior authorization of pharmacy services should be submitted to the CVS/Caremark Utilization Management (UM) Department using one of the following methods:
Turn-Around Times:
Emergency Fills
HSCSN Drug Formulary
Drug Search Example:
![]()